A Devious Cellular Trick Cancers Can Use to Escape Your Immune System
In a surprise discovery, researchers found that cells from some types of cancers escaped destruction by the immune system by hiding inside other cancer cells.
The finding, they suggested in an article published this month in the journal eLife, may explain why some cancers can be resistant to treatments that should have destroyed them.
The research began when Yaron Carmi, an assistant professor at Tel Aviv University, was studying which T cells of the immune system might be the most potent in killing cancers. He started with laboratory experiments that examined treatment-resistant melanoma and breast cancers in mice, studying why an attack by T cells that were engineered to destroy those tumors did not obliterate them.
He was looking at checkpoint inhibitors, a particular type of cancer therapy. They involve removing proteins that ordinarily block T cells from attacking tumors and are used to treat a variety of cancers, including melanoma, colon cancer and lung cancer. But sometimes, after a tumor seems to have been vanquished by T cells, it bounces back.
Dr. Carmi, who loves looking at cells under microscopes, started peering at the tumors while the T cells were attacking them. “I wanted to see the killing, the actual killing,” he said.
Every time, though, he saw some giant cells that remained after the T cells had done their job. “I wasn’t sure what it was, so I thought I would take a closer look,” he said.
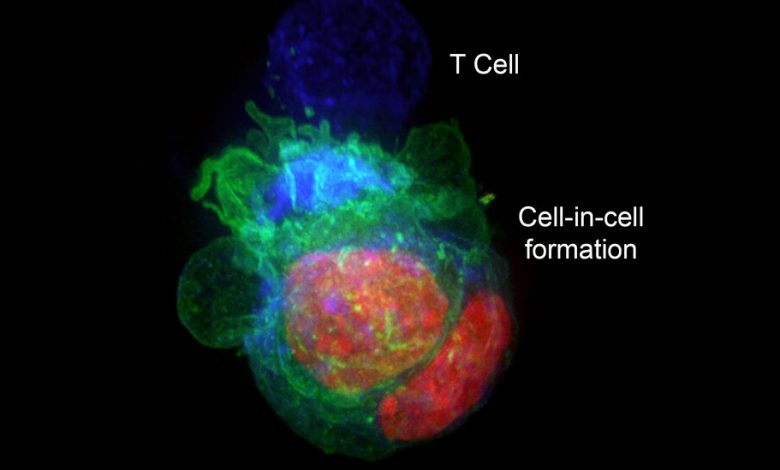
The giant cells turned out to be cancer cells that were harboring other cancer cells, protecting them from destruction. Once the cancer cells escaped to their hiding places, T cells could not get to them, even if the immune system killed the cancer cells that were serving as cellular bunkers.
“It was like seeing the devil,” Dr. Carmi said.
Cancer cells, he added, can remain in hiding “for weeks or months.”
When he removed the T cells from the petri dishes, the cancer cells came out of their shelters.
He looked at human cells from breast cancers, colon cancers and melanomas and saw the same phenomenon. But blood cancers and glioblastomas, the deadly brain cancers, did not form the cell-in-cell structures.
Perhaps, Dr. Carmi reasoned, it might be possible to prevent cancer cells from taking refuge. He decided to examine the genes involved in this defense mechanism. Blocking those genes, he discovered, also blocked the ability of T cells to attack the tumors.
“I realized this is the limit of what the immune system can do,” Dr. Carmi said. “Our immune systems cannot win.”
Others, while fascinated by the discovery, say many questions remain.
“It’s definitely an interesting paper with some strong, compelling observations,” said Dr. Michel Sadelain, an immunologist at Memorial Sloan Kettering Cancer Center, where he heads the center’s gene transfer and gene expression laboratory. But, he asked, how relevant is the finding in disabling immunotherapies in the real world?
Dr. Marcela Maus, the director of the cellular immunotherapy program at the Mass General Cancer Center, said the discovery showed what might be a new cancer cell defense mechanism.
“We have seen that tumors can hide from the immune system, including a kind of ‘impersonating’ immune cells, but I don’t think we’ve ever seen that tumor cells hide inside each other.” But, she added, “I do think it needs to be replicated to gain full traction.”
Dr. Jedd Wolchok, the director of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine, had the same reaction.
“I’ve heard about cancer cells feeding off themselves, feeding off their neighbors, putting out exosomes,” he said, referring to little pouches of signaling chemicals. “I guess this is the next step — hiding inside your neighbor.”
One possible remedy, he said, might be to foil the cancer cells by treating a patient with immunotherapy for a short time, stopping, then treating again. That could be in keeping with new questions about how long patients should be treated with these expensive and toxic drugs. The current advice is to treat for two years. But, Dr. Wolchok said, “many of us are asking, Can you get away with less?”
He cautioned, though, that the immunotherapy the Tel Aviv group had used was not a standard one in cancer patients.
For now, Dr. Wolchok said, while the discovery is “a really innovative observation,” it remains to be seen whether it will lead to improvements in the treatment of cancer patients.